Feeling Nervy? How Cannabis Could Ease Your Nerve Pain

Why Cannabis for Nerve Pain Is Getting Serious Medical Attention
Cannabis for nerve pain has emerged as a promising treatment option for millions of Americans struggling with neuropathic conditions. Research shows that cannabis-based medicines may help 21% of patients achieve significant pain relief compared to 17% with placebo treatments, offering hope where traditional medications often fall short.
Quick Answer for Cannabis & Nerve Pain:
- Evidence: Moderate-quality studies show cannabis can reduce nerve pain by 30-50% in some patients
- Best for: Diabetic neuropathy, HIV-related nerve pain, multiple sclerosis pain
- How it works: THC and CBD interact with your body’s pain receptors and reduce inflammation
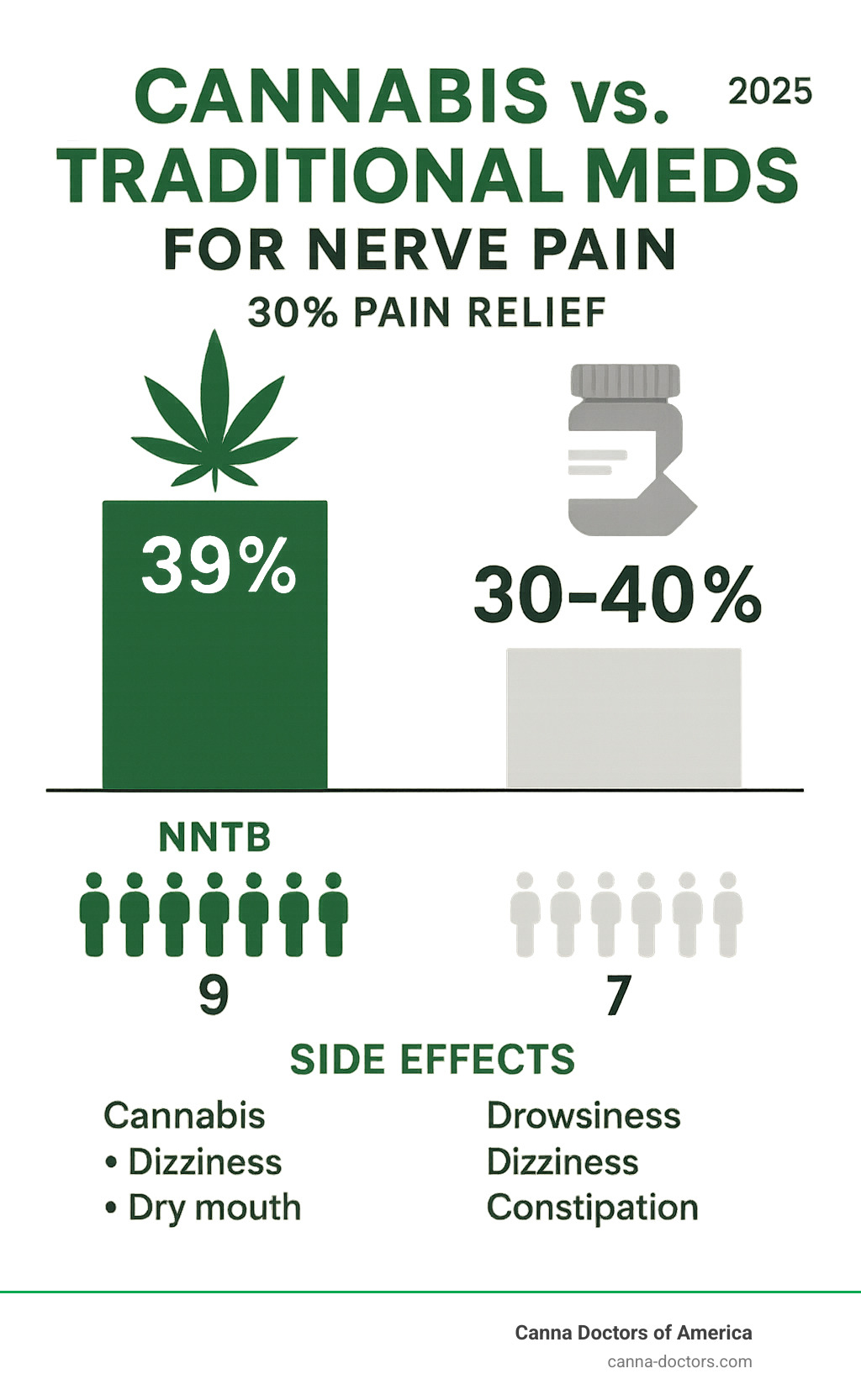
- Common side effects: Dizziness, drowsiness, dry mouth
- Bottom line: May help when standard treatments like gabapentin or duloxetine aren’t enough
Nerve pain – also called neuropathic pain – affects up to 10% of adults and feels different from regular pain. Instead of a dull ache, you might experience sharp, burning, or electric-shock sensations that can make daily life miserable.
The challenge with nerve pain is that it often doesn’t respond well to typical pain relievers. Standard treatments like gabapentin or pregabalin only provide meaningful relief for about 30-40% of patients. This leaves millions searching for alternatives.
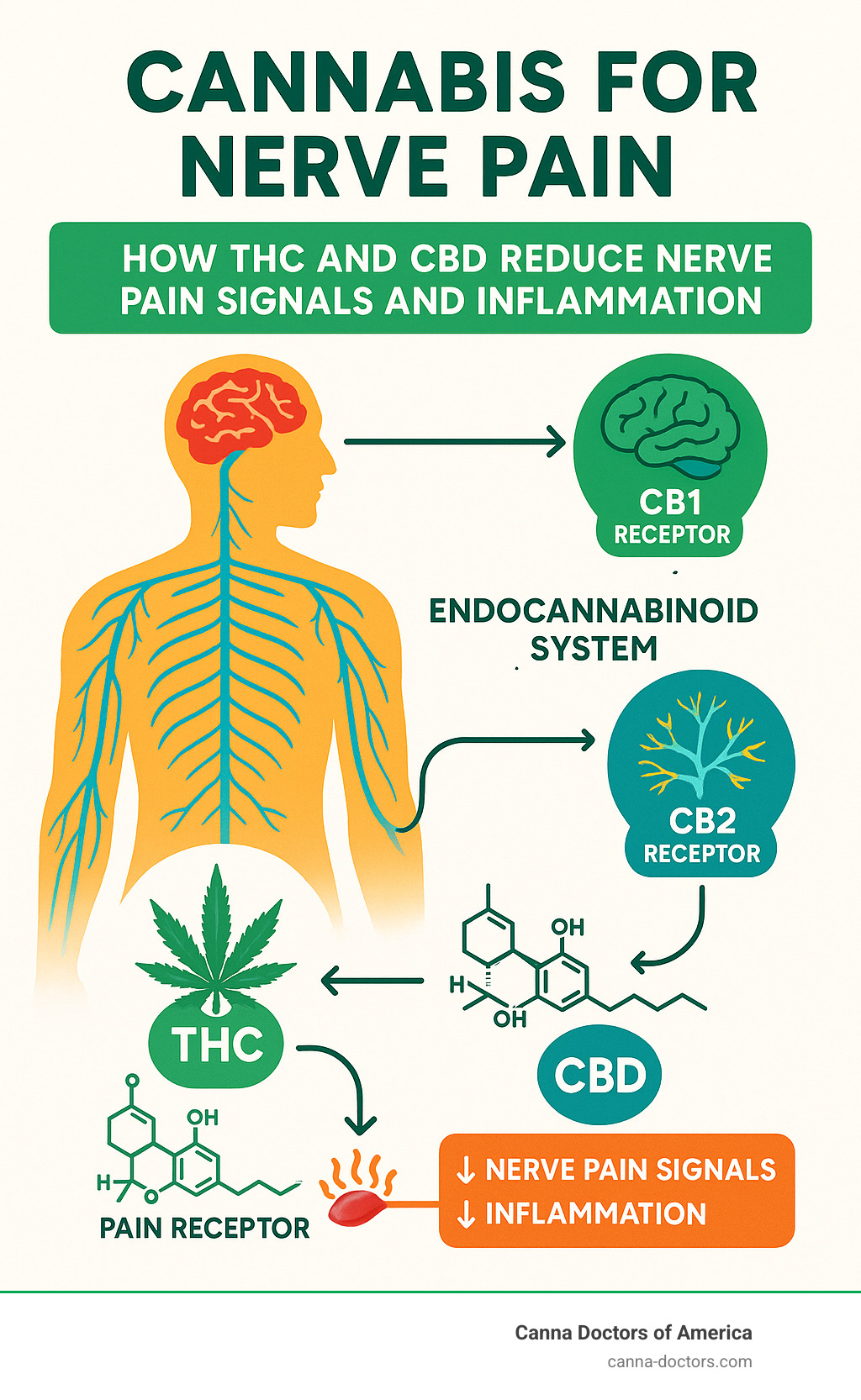
That’s where cannabis enters the picture. Your body has an endocannabinoid system – a network of receptors that help regulate pain, mood, and inflammation. Cannabis compounds like THC and CBD can activate these receptors, potentially offering relief when other treatments fail.
I’m Geoff Massey, Regional Director of Canna Doctors of America, where I’ve helped thousands of patients steer cannabis for nerve pain treatment options. My experience working with medical professionals has shown me how personalized cannabis therapy can transform lives for those suffering from chronic neuropathic conditions.
Cannabis for nerve pain word roundup:
Neuropathic Pain 101: Why Relief Is Hard to Find
Neuropathic pain isn’t like the throbbing you get from a bruise. When nerves are damaged, they misfire, sending phantom pain signals to your brain even when no injury is present. Up to 10 % of adults—about 20 million Americans—live with sensations that range from stabbing shocks to relentless burning or numb-yet-painful tingling.
Diabetes, chemotherapy, shingles, spinal injuries, and multiple sclerosis are the usual suspects, and the discomfort often lingers long after the original problem is treated. As a result, sleep, mood, work performance, and relationships all take a hit, adding billions of dollars in healthcare costs and lost productivity each year.
Current Standard Treatments & Their Limits
Doctors typically start with:
- Gabapentinoids (gabapentin, pregabalin) – calm overactive nerves but only help 30–40 % of patients and can cause dizziness, weight gain, and brain fog.
- Antidepressants (duloxetine, amitriptyline) – alter pain-processing chemicals yet bring nausea or sexual side effects.
- Opioids – risky for dependence and tolerance; not ideal for long-term pain.
- Topicals & procedures – capsaicin, lidocaine, nerve blocks, or spinal cord stimulators can work, but benefits are often modest or temporary.
Even after trying several of these options, two-thirds of people still report inadequate relief. That treatment gap is why more clinicians and patients are turning to cannabis for nerve pain.
Cannabis for Nerve Pain: Mechanism, Product Types & Evidence
To understand how cannabis for nerve pain works, we need to look at a fascinating findy from the late 1980s – your body’s own endocannabinoid system. Think of it as your internal pain management network, complete with two main types of receptors scattered throughout your body.
CB1 receptors live primarily in your brain and nervous system, acting like tiny switches that can dial down pain signals. CB2 receptors hang out mainly in your immune cells and other tissues throughout your body, helping control inflammation and immune responses.
Here’s where it gets interesting. THC (tetrahydrocannabinol) – the compound that creates cannabis’s “high” – fits perfectly into CB1 receptors like a key in a lock. When it binds there, it can potentially reduce those overwhelming pain signals racing through damaged nerves.
CBD (cannabidiol) takes a different approach entirely. This non-intoxicating compound doesn’t create a high, but it works through multiple pathways to reduce inflammation and change how your brain processes pain signals. It’s like having a gentle mediator that helps calm down your overactive pain system.
The “entourage effect” is where things get really fascinating. This theory suggests that cannabis compounds work better as a team than flying solo. It might explain why whole-plant products sometimes outperform isolated compounds – nature’s recipe might be more complex than we initially thought.
Researchers have studied several types of cannabis-based medicines for neuropathic pain, each with its own personality and benefits.
Herbal cannabis – the traditional smoked or vaporized flower – contains the full orchestra of cannabinoids and terpenes. Studies have shown modest but meaningful pain reduction, particularly impressive for HIV-related neuropathy and cases where nothing else worked.
Nabiximols (known as Sativex in many countries) comes as an oromucosal spray with equal parts THC and CBD. It’s already approved in several countries for multiple sclerosis spasticity and has shown real promise in neuropathic pain trials. Each spray delivers a precise dose, making it easier to find your sweet spot.
Synthetic cannabinoids like nabilone and dronabinol are FDA-approved for other conditions but have been studied off-label for pain. They offer the advantage of consistent dosing every time, though they may miss out on that helpful entourage effect.
Research from Scientific research on THC/CBD spray and other clinical trials suggests that cannabis-based medicines can provide meaningful relief for certain types of neuropathic pain, especially when conventional treatments have thrown in the towel.
Does cannabis for nerve pain outperform traditional meds?
The evidence for cannabis for nerve pain tells an encouraging but realistic story. A comprehensive Cochrane review – the gold standard of medical research – analyzed 16 trials with 1,750 patients and found that cannabis-based medicines probably help more people achieve significant pain relief compared to placebo.
The numbers break down like this: 39% of patients using cannabis achieved 30% or greater pain relief, compared to 33% with placebo. For the more demanding 50% pain relief threshold, cannabis still showed benefit with 21% versus 17% with placebo.
To put this in perspective, doctors use something called “Number Needed to Treat” (NNTB) – basically, how many patients you need to treat for one additional person to get meaningful relief. For cannabis achieving 50% pain reduction, the NNTB is 20, meaning you’d need to treat 20 patients for one additional person to achieve significant relief beyond placebo.
How does this stack up against your standard nerve pain medications? The comparison isn’t perfectly apples-to-apples since head-to-head studies are limited, but here’s the honest breakdown:
Pregabalin shows an NNTB of 7-8 for 50% pain relief in diabetic neuropathy, while duloxetine comes in at 5-6 for the same level of relief. Cannabis sits at an NNTB of 20 across various neuropathic conditions.
At first glance, cannabis appears less potent than first-line treatments. But here’s the crucial point – cannabis may shine brightest for patients who haven’t responded to standard medications or can’t tolerate their side effects. It’s not necessarily about being the strongest option; it’s about being an option when other doors have closed.
The evidence quality is rated as moderate to low, which means we need more robust research to draw definitive conclusions. But for patients dealing with treatment-resistant nerve pain, these moderate benefits can feel life-changing.
Product Formats Studied
Researchers have put various delivery methods for cannabis for nerve pain through their paces, each offering different advantages and trade-offs.
Smoked cannabis appeared in several early studies, with patients typically smoking 1-4 times daily. While effective for many, smoking raises obvious respiratory concerns and makes precise dosing about as exact as eyeballing ingredients in grandma’s recipes.
Vaporized cannabis delivers many of smoking’s benefits without the combustion byproducts that worry doctors. Studies have used vaporizers set between 185-210°C (365-410°F) with impressive results for treatment-resistant neuropathic pain. The onset is quick – usually within minutes – making it helpful for breakthrough pain episodes.
Oromucosal sprays like nabiximols provide the consistency that makes doctors happy. Each spray delivers exactly 2.7mg THC and 2.5mg CBD, with patients typically using 2-12 sprays daily. It’s like having a measured medicine dropper for your pain relief.
Oral capsules containing synthetic or plant-derived cannabinoids offer the most precise dosing but require patience. They take 1-3 hours to kick in but then stick around for 6-8 hours, making them better for baseline symptom control than sudden pain flares.
Topical applications with CBD have shown promise for localized neuropathic pain in smaller studies. They work directly where you apply them without affecting your whole system, which appeals to patients worried about cognitive effects.
Dose ranges vary dramatically across studies – from as little as 1mg THC daily to over 20mg. This wide range reflects how individual responses to cannabis can be, emphasizing why personalized dosing is so important. Onset times range from minutes for inhaled products to hours for oral ones, which affects how patients can strategically use these medicines throughout their day.
Risks, Side Effects & Research Gaps
Let’s be honest about the downsides of cannabis for nerve pain – because understanding the risks is just as important as knowing the benefits.
The most common side effects aren’t dangerous, but they can definitely affect your daily life. Dizziness tops the list, affecting up to 61% of cannabis users compared to just 29% of people taking placebo in studies. That’s a significant difference that could impact your ability to drive or work safely.
Drowsiness and fatigue are also frequent complaints, along with dry mouth and nausea. Some patients experience what researchers call “cognitive impairment” – basically feeling foggy or having trouble concentrating. These effects are usually temporary and fade as your body adjusts, but they’re worth planning for.
The psychiatric effects deserve special attention. About 17% of cannabis users in studies experienced mood changes, anxiety, or paranoia, compared to only 5% taking placebo. While rare, some people can have more serious reactions like panic attacks or, in very uncommon cases, psychotic episodes. This is why mental health screening is so important before starting treatment.
Here’s a sobering statistic: 10% of patients stopped using cannabis due to side effects, compared to 5% who stopped taking placebo. That means for every 25 people who try cannabis for nerve pain, one additional person will quit because of adverse effects they couldn’t tolerate.
Long-term safety is where things get murky. Most studies only lasted 2-15 weeks, so we’re essentially flying blind when it comes to what happens after months or years of use. This is concerning because many nerve pain patients need ongoing treatment.
Potential long-term worries include lasting cognitive effects (especially with high-THC products), respiratory problems from smoking or vaping, and the possibility of developing problematic use patterns. About 10% of regular cannabis users develop what doctors call “cannabis use disorder” – essentially becoming dependent on the medication.
Drug interactions are another blind spot. Cannabis can affect how your liver processes other medications, potentially making them stronger or weaker. This is particularly important if you’re taking blood thinners, seizure medications, or heart drugs.
The research itself has some significant limitations that affect how we interpret results. Most studies excluded people with substance abuse history, psychiatric disorders, heart conditions, or those who were pregnant. This means the research might not reflect how cannabis works in the real world for people with complex medical histories.
Additionally, many studies used lower-potency cannabis than what’s available in today’s dispensaries. Modern products can be much stronger, which could mean both better pain relief and more side effects than the research suggests.
The bottom line? Researchers rate the evidence quality as “very low to moderate,” meaning future studies could significantly change our understanding of both benefits and risks. That’s why working with experienced medical professionals is crucial when considering cannabis for nerve pain treatment.
Getting Started with Medical Cannabis: Practical Steps & Eligibility
Florida’s medical cannabis program is straightforward, and Canna Doctors of America guides you from start to finish at our Tampa, St. Petersburg, and Clearwater clinics.
- Physician evaluation – A qualified doctor reviews your history and confirms you have chronic neuropathic pain that hasn’t responded to standard care.
- State registration – We submit everything to the Office of Medical Marijuana Use. Most patients receive an email approval in 5–10 business days; your physical card follows by mail.
- Dispensary visit – Use your card to purchase lab-tested products at any licensed dispensary in Florida.
Same-day in-office approval is available for many patients, and we provide clear dosing instructions so you leave knowing exactly how to start.
Who Qualifies?
Florida lists chronic non-malignant pain—including diabetic neuropathy, post-chemo pain, multiple sclerosis pain, and other neuropathies—as a qualifying condition when conventional therapies have failed. You must:
- Be a Florida resident with valid ID
- Provide records confirming your diagnosis and past treatments
- Complete a brief mental-health and contraindication screen (e.g., active substance misuse, uncontrolled psychosis, certain cardiac issues, pregnancy)
Safe Dosing & Monitoring
“Start low, go slow” really works:
- THC: begin with 1–2.5 mg daily, increase every few days as needed
- CBD: start around 5–10 mg daily; higher doses are generally well-tolerated
Choose the route that fits your lifestyle:
- Sublingual tinctures – 15–45 min onset, 2–4 h duration
- Vaporized flower/oil – 2–15 min onset, 1–3 h duration (great for breakthrough pain)
- Edibles – 30–120 min onset, 4–8 h duration (ideal for nighttime)
- Topicals – localized effect without intoxication
Avoid driving while impaired, store products safely, and tell all healthcare providers about your cannabis use to prevent drug interactions (especially with blood thinners, seizure, or heart medications).
Record your doses, pain scores, and side effects in a simple journal or phone app—small adjustments based on these notes often make the difference between partial and meaningful relief.
For more details, visit our Florida medical cannabis approval page.
Conclusion
Chronic nerve pain can feel endless, but it doesn’t have to dictate your life. While cannabis isn’t a cure-all, studies—and our real-world experience—show it can offer meaningful relief, especially when first-line drugs fall short.
If you’re ready to explore a researched, physician-guided option, Canna Doctors of America is here to help you secure your card, tailor a safe dosing plan, and track your progress—all in a single, streamlined visit.
Take the next step toward better sleep, improved mood, and manageable pain. Learn more or schedule your consultation at our Tampa, St. Petersburg, or Clearwater clinics by visiting our Florida medical cannabis approval page today.