Pain, Pain Go Away – Medical Marijuana to Save the Day

Why Medical Marijuana for Chronic Pain is Gaining Medical Attention
Medical marijuana for chronic pain is increasingly recognized as a viable alternative to traditional pain medications. While research is ongoing, studies show substantial support for its use in treating neuropathic pain and helping reduce opioid dependence.
Quick Facts About Medical Marijuana for Chronic Pain:
- Evidence Level: Substantial evidence for neuropathic pain; limited for other chronic pain types.
- Opioid Reduction: Studies show a 44-64% reduction in opioid use when combined with medical cannabis.
- Safety Profile: No recorded overdose deaths, compared to 75% of drug overdoses involving opioids in 2021.
- Patient Preference: 81% of patients using both cannabis and opioids report cannabis is more effective alone.
- Common Conditions: Most effective for nerve damage pain, multiple sclerosis spasticity, and cancer-related pain.
Chronic pain affects over 50 million Americans. With the opioid crisis claiming hundreds of thousands of lives, patients and doctors are seeking safer alternatives. Medical cannabis works with the body’s endocannabinoid system, offering a different approach than simply masking pain signals.
Research highlights its potential: a CUNY study found that long-term medical cannabis use led to 51% reductions in daily opioid doses. A Finnish study revealed that cannabis users reported not just pain relief but also improved mood and sleep compared to opioid users.
However, cannabis is not a cure-all. Evidence varies by pain type, and combining it with opioids can carry risks. I’m Geoff Massey, Regional Director of Canna Doctors of America. I help patients steer medical marijuana for chronic pain through proper medical guidance. I’ve seen how the right, medically-supervised approach can transform lives when other treatments have failed.
Industry Snapshot: In Florida alone, several physician groups now focus on medical cannabis certificationincluding DocMJ, Green Health Docs, Compassionate Care Clinics, and my own Canna Doctors of Americaso patients have multiple choices for evidence-based guidance. While each clinic has a slightly different intake process and fee structure, all of them operate under the same state rules, evaluate qualifying conditions, and submit the required documentation to the Office of Medical Marijuana Use. Comparing services, hours, follow-up policies, and telehealth availability can help you decide which provider best fits your needs.
Medical marijuana for chronic pain terms explained:
The Science Behind Cannabis for Pain: What Does the Research Say?
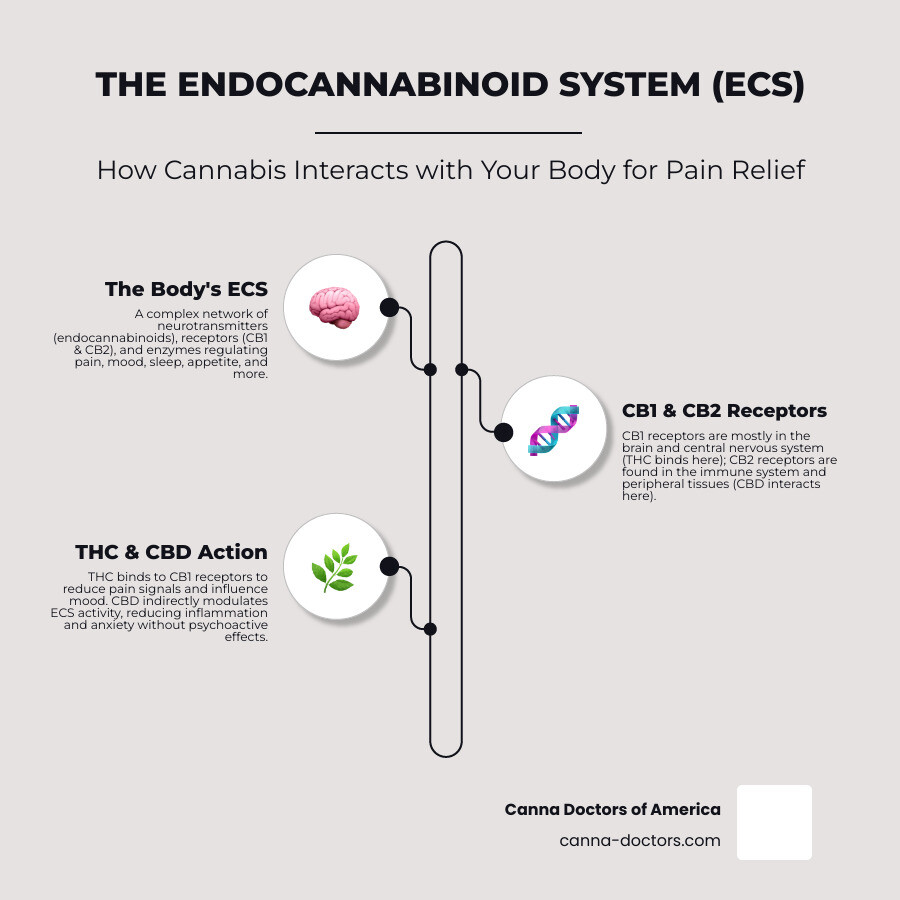
For thousands of years, cannabis has been used for its medicinal properties. Today, modern science is helping us understand how it works. The key is the body’s endocannabinoid system (ECS), a communication network that helps regulate mood, sleep, appetite, and pain. Cannabis contains compounds called cannabinoids (like THC and CBD) that interact with ECS receptors to influence these functions.
The evidence for cannabis in treating chronic pain is evolving. While it’s not a blanket solution for all pain, its effectiveness in specific conditions is gaining strong scientific backing. For instance, The National Academies of Sciences report on cannabis health effects [https://nap.nationalacademies.org/catalog/24625/the-health-effects-of-cannabis-and-cannabinoids-the-current-state.] found substantial evidence that cannabis is an effective treatment for chronic pain, particularly for nerve pain, multiple sclerosis-related spasms, and chemotherapy-induced nausea.
THC vs. CBD for Pain Relief
When discussing medical marijuana for chronic pain, the two main cannabinoids are THC (tetrahydrocannabinol) and CBD (cannabidiol). They both help with pain but work differently.
THC is the primary psychoactive component, responsible for the “high.” It activates the brain’s reward system, which can reduce pain perception and improve mood. For many, this effect is part of the therapy, helping them relax and dissociate from their pain.
CBD is non-psychoactive and celebrated for its anti-inflammatory properties. CBD’s non-psychoactive anti-inflammatory properties make it a great option for patients seeking pain relief without the cognitive effects of THC.
The ratio of THC to CBD is critical. Some patients benefit from a balanced ratio, while others, especially new users, may prefer high-CBD products. This highlights why consulting a doctor is essential to find the personalized formulation that works for your body and your pain.
The Evidence for Specific Pain Types
While evidence is limited for some pain types, research into medical marijuana for chronic pain shows great promise in specific areas.
Neuropathic pain (pain from nerve damage) is one of the most well-supported uses. A 2015 review confirmed its effectiveness for neuropathy [https://www.ncbi.nlm.nih.gov/pubmed/26103031], a condition that is often difficult to treat.
Beyond neuropathy, cannabis has shown potential for other conditions. One study found that cancer patients using cannabis reduced their opioid use by 64%. Similarly, some people with chronic migraines report fewer episodes after using cannabis.
However, the results are not always consistent. A 2018 Australian study on recreational users found cannabis did not reduce pain or the need for opioids. Such varying outcomes underscore the need for more targeted research, particularly focusing on medically supervised use versus recreational use.
For specific conditions, the evidence for medical marijuana for chronic pain is compelling, but more research is needed to clarify its role across the full spectrum of pain management.
A Potential Alternative? Medical Marijuana for Chronic Pain vs. Opioids
The opioid crisis is a stark reminder of the dangers of traditional pain management. In 2021, over 106,000 Americans died from drug overdoses, with opioids involved in 75% of those deaths. While effective for short-term pain, opioids carry a high risk of addiction and severe side effects with long-term use.
This is why many are turning to medical marijuana for chronic pain, which offers a much better safety profile. Critically, there has never been a recorded fatal overdose from cannabis alone, a stark contrast to opioids, where the line between therapeutic and lethal doses is dangerously thin.
Patient experience supports this shift. In one survey of people who used both substances, 81% said cannabis was more effective when used alone, and 97% believed they could reduce their opioid use with access to cannabis. At medical cannabis clinics, patients often report not just pain relief but also better sleep, improved mood, and a feeling of reclaiming their lives.
The Impact of Medical Cannabis on Opioid Use
One of the most promising areas of research is how medical marijuana for chronic pain helps people reduce opioid dependence.
A groundbreaking CUNY study on opioid dosage reduction found that patients using medical cannabis for over 30 days significantly lowered their opioid doses. The study showed that patients on higher initial opioid doses saw the largest reductions. Those taking 90 MME (morphine milligram equivalents) or more daily reduced their opioid use by up to 51%.
This means people on high doses of painkillers could potentially cut their intake in half while still managing their pain—a life-saving prospect. On a broader scale, states with medical cannabis programs have seen reductions in overall opioid prescriptions, suggesting cannabis can be a valuable harm reduction tool.
Understanding the Benefits of Using Medical Marijuana for Chronic Pain
The benefits of medical marijuana for chronic pain extend beyond simple pain scores. The most significant advantage is fewer dangerous side effects. Unlike opioids (risk of respiratory depression, addiction) or NSAIDs (risk of stomach bleeding, liver damage), cannabis has a gentler profile with no risk of fatal overdose.
Cannabis can also lead to reduced reliance on multiple medications. Many chronic pain patients take a cocktail of drugs for pain, sleep, and anxiety. Cannabis may help simplify this regimen.
Perhaps the most meaningful benefit is improved overall well-being. A Finnish study found that while cannabis and opioid users experienced similar pain reduction, the cannabis users reported significantly better mood, sleep, and functionality. They felt more relaxed and better able to cope with their pain by changing their relationship to it, allowing them to “feel pain without reacting negatively to it.”
Weighing the Risks of Combining Cannabis and Opioids
While cannabis can help reduce opioid use, combining these substances is complex and requires caution. Research shows that for some individuals, combining cannabis with opioids can increase the risk for opioid misuse. This seeming contradiction highlights how responses vary from person to person.
Combining substances can be unpredictable, particularly for those with a predisposition to substance use disorders. What works as harm reduction for one person might create new problems for another.
This is why medical supervision is absolutely crucial. Contradictory study results often reflect the difference between medically guided use and self-medication. Experience from specialized clinics, including Canna Doctors of America, shows that when patients work with knowledgeable providers to transition carefully, the results can be transformative. Trying to manage this combination alone is risky.
The bottom line: this is not a DIY situation. Any decision to use cannabis alongside or in place of opioids must be made with a healthcare provider who understands both substances and your medical history.
How to Use Medical Cannabis for Pain Relief
If you’re considering medical marijuana for chronic pain, the next step is to approach it like any other serious health decision: with professional guidance. A qualified physician can assess your specific condition, review other medications, and recommend the right type, dose, and method of cannabis for you.
Navigating the legal requirements is also key. Rules vary by state, but in Florida, specialized physician groups like Canna Doctors of America, DocMJ, and Green Health Docs help patients understand the program and obtain a medical marijuana card if they qualify. For a broader look, you can find an overview of state medical marijuana laws online.
Cannabis Strains: Indica, Sativa, and Hybrids
You’ll often hear terms like “Indica” for relaxation and “Sativa” for energy when discussing medical marijuana for chronic pain. Many patients find these classifications helpful, with one survey showing a preference for Indica strains for pain management and sleep [https://www.liebertpub.com/doi/abs/10.1089/acm.2013.0190].
However, the science is not so clear-cut. There is little medical evidence that these labels reliably predict effects. A strain’s impact comes from its unique combination of hundreds of compounds, including cannabinoids (THC, CBD) and terpenes—a concept known as the “entourage effect.”
This is why personalized medical advice is vital. The right product for one person’s back pain may not work for another’s nerve pain. A qualified physician will work with you to understand your needs and guide you to the right product, regardless of its strain classification. It’s about finding what truly works for you.
Methods of Administration
One of the great things about medical marijuana for chronic pain is the variety of non-smoking options available, allowing you to get therapeutic benefits without the risks of smoke inhalation.
- Edibles: These cannabis-infused products (gummies, chocolates) offer discreet, long-lasting relief. Effects can take 30-120 minutes to begin.
- Tinctures and Oils: Placed under the tongue, these liquid extracts offer fast-acting (15-45 minutes) and precise dosing.
- Topicals: These cannabis-infused lotions and balms are applied directly to the skin for localized pain and inflammation relief without psychoactive effects.
- Transdermal Patches: Like a nicotine patch, these deliver a slow, steady dose of cannabinoids through the skin for consistent, long-term relief.
- Vaporizing: This method heats cannabis to release a vapor without the harmful byproducts of smoke. It offers a fast onset of effects with less lung irritation than smoking.
Choosing the right method depends on your pain type, desired onset and duration of relief, and personal preference. A qualified medical professional can help you select the best approach for your pain management plan.
Navigating the Risks and Legal Landscape
While medical marijuana for chronic pain is promising, understand the potential risks and the complex legal environment. Like any medical treatment, it’s about making informed choices.
Potential side effects are typically mild and dose-dependent, including dizziness, nausea, dry mouth, or red eyes. Higher THC doses may cause temporary anxiety or paranoia. Our goal is to find a dose that minimizes these effects.
A more serious concern is cannabis use disorder (CUD), the clinical term for addiction. While less common and severe than opioid addiction, it is a real risk. About 10% of cannabis users may develop CUD, with higher risks for those who start young or use daily. Withdrawal symptoms can include irritability, anxiety, and sleep disturbances. This is why professional guidance and monitoring are critical. You can learn more from the National Library of Medicine’s resource on cannabis use disorder.
The legal landscape is complicated. Federally, cannabis remains a Schedule I drug, classified as having “no currently accepted medical use and a high potential for abuse.” This creates challenges for research. However, many states, including Florida, have legalized medical cannabis. The 2018 Farm Bill legalized industrial hemp (cannabis with very low THC), but products with higher THC content remain federally illegal, even if they are legal under a state’s medical program.
The FDA has approved a few synthetic cannabinoids (dronabinol, nabilone) and one plant-derived drug (Epidiolex) for specific conditions. Please note, these are lab-developed pharmaceuticals. Canna Doctors of America does not offer or recommend these synthetic cannabinoids. Our focus is on providing physician-guided access to state-legal, whole-plant medical cannabis in full compliance with Florida’s program.
Frequently Asked Questions about Medical Marijuana for Chronic Pain
Patients considering medical marijuana for chronic pain often have similar questions. Here are honest answers to the most common ones we hear at our clinics in Tampa, St. Petersburg, and Clearwater.
Is medical marijuana more effective than opioids for pain?
It’s not a simple yes or no. For certain conditions, especially neuropathic (nerve) pain, studies show medical marijuana for chronic pain can be as effective as opioids, but with a much better safety profile. Cannabis has never caused a fatal overdose, making it a compelling option for long-term management.
Patients also report better quality of life, including improved mood and sleep. However, for some types of severe, acute pain, opioids may still be necessary. The goal is often to use cannabis as a tool to reduce reliance on more dangerous medications, not always to replace them entirely. Effectiveness depends on the individual, their pain type, and a medically supervised treatment plan.
What type of cannabis is best for chronic pain?
While many patients prefer relaxing “Indica” strains for pain, science shows it’s more complex. There’s no consensus that strain names predict effects. The key is the specific ratio of cannabinoids like THC and CBD. What works is highly individual, depending on your body chemistry and pain type.
This is why a doctor’s recommendation is crucial to find the right chemical profile for you, rather than relying on dispensary marketing terms. A qualified physician will work with you, starting with low doses and adjusting to find what works best for your body and your pain.
Can I get addicted to medical marijuana?
Yes, the risk of cannabis use disorder (CUD) is real, though it is significantly lower than with opioids. Research suggests about 10% of cannabis users may develop CUD, with higher risks for those who start young or use daily.
It’s important to distinguish between dependence (physical adaptation, causing mild withdrawal if stopped suddenly) and addiction (compulsive use despite negative consequences). Under medical supervision, most patients use cannabis responsibly to improve their lives. We monitor for any signs of problematic use and adjust treatment as needed.
If you have concerns about addiction, talk to your doctor. Resources are available, including SAMHSA’s National Helpline (1-800-662-HELP) and their treatment locator. With proper medical guidance, you can use medical marijuana for chronic pain safely and effectively.
Conclusion
Living with chronic pain is a battle, but medical marijuana for chronic pain offers real, science-backed hope. We’ve seen that cannabis is a legitimate medical option that is changing lives.
The research is compelling. For conditions like neuropathic pain, the evidence is substantial. Cannabis’s ability to help patients reduce opioid dependence—by up to 51% in some studies—is a potential breakthrough, especially given the dangers of the opioid crisis.
Medical marijuana for chronic pain works with your body’s natural endocannabinoid system to help regulate pain and mood. It supports what your body already knows how to do.
But here’s the most important takeaway: success with medical cannabis comes from treating it as medicine. The patients who find the most relief work with qualified physicians to find the right products, dosages, and methods for their specific needs.
If you’re ready to explore if medical cannabis can help you, the next step is to consult with a qualified provider. In Florida, numerous clinics, including our team at Canna Doctors of America serving Tampa, St. Petersburg, and Clearwater, can walk you through the state’s medical marijuana program and determine if cannabis is right for you.
Learn how to get your medical marijuana card in Florida and find if medical marijuana for chronic pain could be the missing piece in your pain management puzzle. You deserve to live with less pain.