Fibromyalgia Pain Relief Explained: Treatments That Actually Help

Understanding Fibromyalgia: The Challenge of Widespread Pain
Fibromyalgia chronic pain relief is a primary goal for the millions of Americans living with this complex condition. The most proven approaches include:
Most Effective Fibromyalgia Pain Relief Methods:
- Exercise therapy – Aerobic and strength training (reduces pain by 30-40%)
- FDA-approved medications – Pregabalin, duloxetine, and milnacipran
- Cognitive Behavioral Therapy (CBT) – Helps change pain perception
- Medical cannabis – Shows promise for pain and sleep improvement
- Acupuncture – Effects can last up to 3 months
- Combination approach – Multiple treatments work better than single therapy
Fibromyalgia is a chronic condition causing widespread pain, affecting 1-5% of the population, most commonly women between 20 and 50.
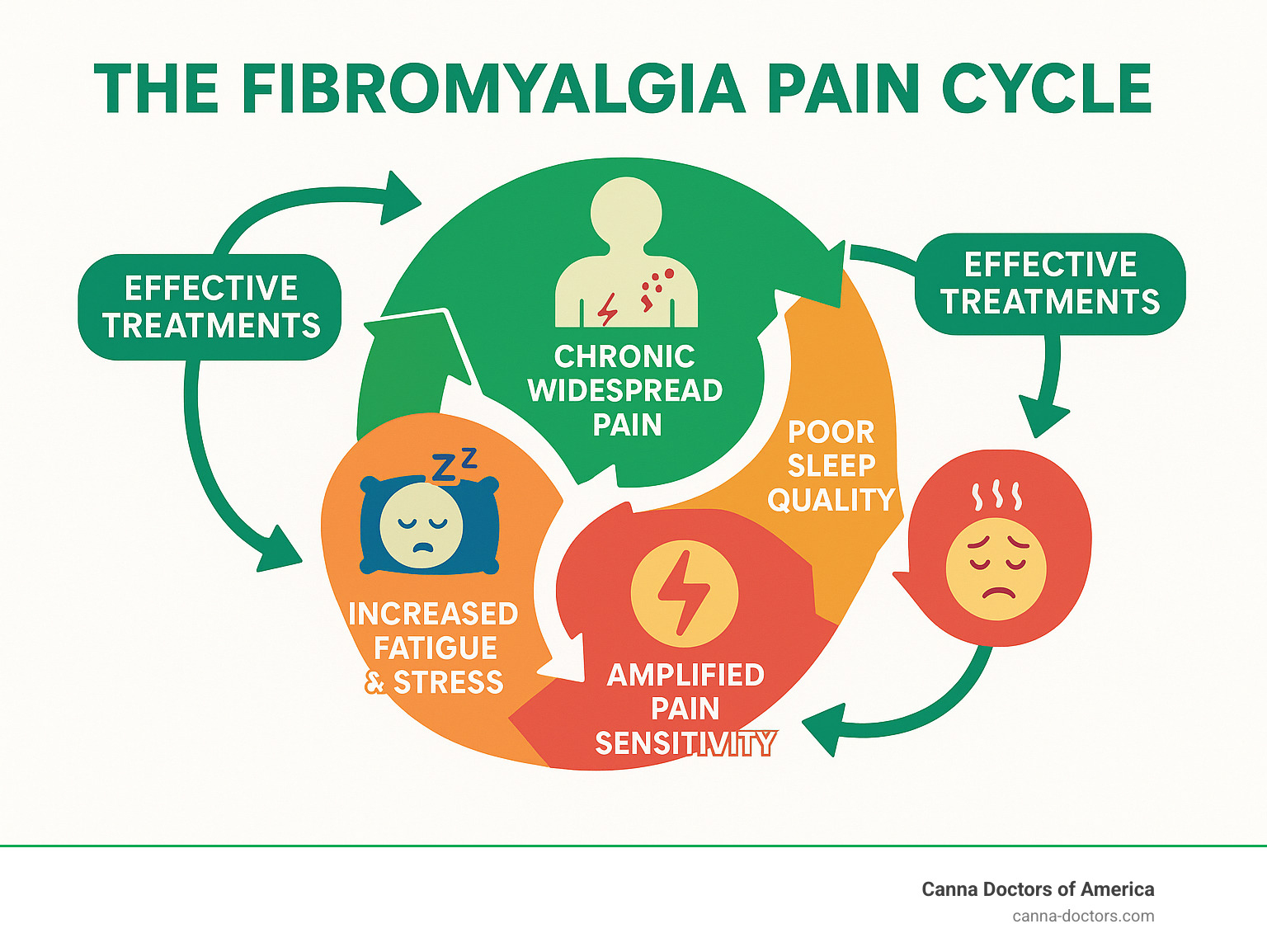
The condition involves three main problems:
- Central sensitization – Your nervous system becomes oversensitive to pain signals.
- Sleep disruption – Poor sleep worsens pain, creating a vicious cycle.
- “Fibro fog” – Memory and concentration problems that impact daily life.
Unlike arthritis, fibromyalgia pain stems from how the brain processes signals, which is why traditional pain medications are often ineffective.
The good news is that research shows a multi-faceted approach provides the best results. While no single treatment works for everyone, the right combination can significantly improve your quality of life.
I’m Geoff Massey, Regional Director of Canna Doctors of America. I help patients explore treatment options, including medical cannabis for fibromyalgia. I’ve seen how combining the right treatments can transform lives when conventional methods fail.
Fibromyalgia chronic pain relief vocab to learn:
Building a Foundation: Non-Pharmacological Pain Relief
Your journey to fibromyalgia chronic pain relief should begin with a non-drug foundation. While medications can be helpful, they only work for about 30-50% of patients alone. The best results come from combining approaches.
This foundation starts with understanding your condition and actively participating in your care. Patient education is a powerful tool. Understanding why you have pain and how treatments work empowers you to take control. Research shows the effectiveness of health education for fibromyalgia patients improves outcomes and reduces anxiety.
Self-management means learning to read your body’s signals, identify flare triggers, and develop personal strategies. It’s about becoming an expert on your fibromyalgia.
Surprisingly, physical activity is one of the most effective treatments for fibromyalgia. Even when you feel you can’t, gentle, consistent movement is a game-changer. Start slow and build gradually—a gentle walk, not a marathon.
The key is consistency over intensity. Your body needs time to adapt, so pushing too hard will likely backfire. Your new motto is “start low and go slow.”
The Role of Exercise and Physical Therapy
Exercise works so well for fibromyalgia because it does several things at once: it releases endorphins (your body’s natural painkillers), improves sleep, boosts mood, and changes how your nervous system processes pain.
Studies with over 2,400 patients show that aerobic exercise can decrease pain, improve physical function, and reduce fatigue. The evidence for aerobic exercise in managing fibromyalgia is solid. Aerobic activities like walking, swimming, or biking are excellent starting points. Even five minutes of walking is a victory.
Strength training doesn’t require heavy weights. Simple resistance exercises with your body weight or light weights can improve muscle function and reduce stiffness. A certified trainer can help you learn safe movements.
Water-based exercise is often a revelation. The water’s buoyancy supports your body, reducing stress on painful joints and allowing for greater movement. Many patients find they can move without the usual pain.
Physical therapy provides professional expertise for your movement journey. A physical therapist who understands fibromyalgia can help you improve range of motion, develop proper body mechanics, and create a custom exercise program. They can also teach you techniques for managing flares.
Psychological Therapies for Managing Pain Perception
Fibromyalgia involves a complex mind-body connection. Your brain’s pain processing system becomes oversensitive. Psychological therapies help reset this system.
Many patients struggle with pain catastrophizing—where the brain expects the worst from any pain signal. This is a neurological response that intensifies pain.
Cognitive Behavioral Therapy (CBT) helps you identify and change negative thinking that worsens pain perception. CBT for fibromyalgia has shown superior results for reducing short-term pain. It gives you practical tools for daily use.
Acceptance and Commitment Therapy (ACT) helps you accept pain as part of your reality while committing to actions that improve your life despite it. It’s about redirecting energy toward what you can control.
Mindfulness practices can be powerful for fibromyalgia chronic pain relief. Focusing on the present moment changes how your brain processes pain. Studies show mindfulness can reduce stress, depression, and anxiety. Apps like Calm or Headspace are great for starting.
Stress reduction is crucial, as stress fuels fibromyalgia. Techniques like deep breathing, meditation, or biofeedback can significantly reduce stress’s impact on your pain.
Connecting with others who understand is also powerful. Local support groups provide emotional support and practical tips. You can connect with others via the Arthritis Foundation or find fibromyalgia-specific groups in your area.
Building this foundation takes time and patience. The goal is to create a toolkit of strategies that work together to give you more control over your symptoms.
A Guide to Medications for Fibromyalgia Chronic Pain Relief
When lifestyle changes and therapy aren’t enough, medications can be a crucial part of your fibromyalgia chronic pain relief strategy. There’s no magic pill for fibromyalgia, but the right medication can significantly reduce pain, improve sleep, and boost energy.
Medications are one tool, not the whole solution. They work best combined with exercise and stress management. Finding the right fit requires patience and collaboration with your doctor.
FDA-Approved Medications for Fibromyalgia
Three medications are specifically FDA-approved for fibromyalgia, accounting for about 70% of all prescriptions.
Pregabalin (Lyrica) was the first medication approved for fibromyalgia. It works by calming overactive nerve signals in the brain and spinal cord. For every 4 to 14 people who try it, one will experience at least 50% pain reduction—meaningful odds for many patients.
Duloxetine (Cymbalta) increases levels of serotonin and norepinephrine, brain chemicals that regulate both pain and mood. Many patients find it addresses both physical pain and the depression that often accompanies chronic illness.
Milnacipran (Savella) works similarly to duloxetine by balancing the same brain chemicals. Some people respond better to one than the other, so your doctor may try both to see which is more effective for you.
These medications address the central sensitization at the heart of fibromyalgia, helping to normalize how your brain processes pain signals.
Off-Label Medications and Their Effectiveness
Doctors often prescribe medications “off-label,” meaning they are approved for other conditions but have proven helpful for fibromyalgia.
Antidepressants were used for fibromyalgia long before there were FDA-approved options. Older tricyclic antidepressants like amitriptyline can be very effective, reducing Fibromyalgia Impact Questionnaire scores by 30% in studies. A comparison of Amitriptyline and FDA-approved treatments shows it holds its own against newer drugs.
Amitriptyline often helps with sleep problems, which can break the vicious cycle of pain and poor sleep. Its sedative effect can be therapeutic for fibromyalgia patients.
Other SNRIs like venlafaxine and SSRIs like fluoxetine (Prozac) are also used. Your doctor might choose one based on your main symptoms, such as picking a less sedating option if fatigue is your biggest issue.
Gabapentin, another anti-epileptic medication like pregabalin, works on similar nerve pathways and is another option if pregabalin doesn’t work for you.
Medications to Approach with Caution
Not all pain medications are suitable for fibromyalgia chronic pain relief. Some can make things worse.
Opioids are a major concern. They generally don’t work well for fibromyalgia, carry serious risks of dependence, and can even increase pain sensitivity over time.
NSAIDs like ibuprofen are for inflammatory pain, but fibromyalgia is not an inflammatory condition. A Cochrane review on NSAIDs confirms their limited effectiveness for fibromyalgia.
Benzodiazepines like Xanax might seem helpful for anxiety or sleep, but they can interfere with deep sleep stages and carry dependence risks.
Corticosteroids like prednisone are powerful anti-inflammatories, but they are not effective for fibromyalgia pain and have significant side effects.
Finding the right medication often takes time and patience. Work closely with your doctor to find your personal winning combination.
Exploring Complementary and Emerging Treatments
When traditional treatments aren’t providing enough fibromyalgia chronic pain relief, it’s time to explore integrative medicine. This holistic approach combines conventional treatments with complementary therapies that address the mind-body connection.
This approach recognizes that fibromyalgia affects your entire life—sleep, mood, energy, and relationships. Addressing these interconnected pieces often yields better results than single-focus treatments.
Always discuss new therapies with your healthcare provider before starting them, as some can interact with medications or may not be appropriate for you.
Hands-On and Mindful Therapies for Fibromyalgia Chronic Pain Relief
These therapies directly address pain, muscle tension, and stress.
Acupuncture has helped manage pain for thousands of years. Research shows acupuncture for fibromyalgia can provide relief that lasts up to 3 months post-treatment by stimulating nerves and improving blood flow.
Massage therapy, especially techniques like myofascial release, works on tight, painful muscle knots. It reduces muscle tension, improves circulation, lowers stress hormones, and often improves sleep.
Yoga and Tai Chi combine gentle movement with mindfulness, making them ideal for fibromyalgia. They improve mood, reduce fatigue, and lessen pain. A 2018 study on Tai Chi effectiveness found it produced similar or greater improvement in symptoms than aerobic exercise.
Cryotherapy (cold therapy) can provide significant relief. Applying a cold pack for ten minutes can numb nerve endings and reduce pain for up to twenty-four hours.
Diet, Supplements, and Other Emerging Options for Fibromyalgia Chronic Pain Relief
What you eat can significantly impact your symptoms. An anti-inflammatory diet rich in fruits, vegetables, and healthy oils often helps. Some patients find relief by identifying food sensitivities through an elimination diet.
Several supplements show promise for fibromyalgia chronic pain relief. Vitamin D deficiency is common and linked to increased pain; supplementation can help. Magnesium and B vitamins are also recommended for nerve function and energy. Other supplements being explored include Chlorella, CoQ10, and Acetyl-L-carnitine. A dietary interventions review offers more insight.
Low-Dose Naltrexone (LDN) is an emerging treatment that reduces neuroinflammation. Studies show it can reduce pain scores compared to a placebo.
Medical Cannabis is one of the most promising emerging treatments. It interacts with the body’s endocannabinoid system to help regulate pain, sleep, and mood. Patient satisfaction is notably high; one survey found 62% of users rated it “very effective,” compared to 10% for Lyrica and 8% for Cymbalta. Research on cannabis for treating fibromyalgia shows a combination of THC and CBD is typically more effective than CBD alone.
Other emerging treatments include infrared sauna therapy, green light therapy, neurofeedback, Calmare Scrambler Therapy, and ketamine infusions for treatment-resistant cases.
The key is finding the right combination of treatments for you. Patience and persistence are essential as you explore these options with your healthcare team.
Creating Your Personalized Fibromyalgia Treatment Plan
The truth about fibromyalgia chronic pain relief is that there’s no one-size-fits-all solution. Fibromyalgia affects everyone differently, so your treatment plan must be personalized.
Creating your plan is like solving a puzzle. It involves trial and error with different treatments—exercise, medication, acupuncture—to find what works. While potentially frustrating, this process is key to finding effective relief.
Having the right team is crucial. Your healthcare team might include your primary care doctor, a rheumatologist, a physical therapist, and pain specialists. Each brings a different expertise to the table.
You are the most important member of your healthcare team. Your daily experiences and insights are invaluable for guiding treatment decisions.
Tracking Symptoms and Progress
To find effective fibromyalgia chronic pain relief, tracking your symptoms is essential. It’s like having a roadmap that helps you see patterns you might otherwise miss.
Symptom journaling can reveal connections between your pain and certain foods, activities, or stress levels. Track your daily pain levels (on a 0-10 scale), fatigue, sleep quality, and potential triggers like stress or weather changes.
Professional tools can help. The Visual Analogue Scale (VAS) provides a consistent way to measure pain, while the Fibromyalgia Impact Questionnaire (FIQ) assesses how symptoms affect your daily life. Having baseline measurements helps track real progress.
A downloadable Sample Fibromyalgia Symptom Log (PDF) can help you start with a proven format.
This detailed record is invaluable during doctor visits, providing concrete data to show which treatments are working.
Long-Term Management and Adjusting Your Approach
Fibromyalgia is a dynamic condition, meaning your symptoms will fluctuate. You may have good weeks followed by flare-ups. This is normal and doesn’t mean your treatment has failed.
Your treatment approach must also be flexible. What provides excellent fibromyalgia chronic pain relief during a calm period may need adjustment during a flare. Your exercise routine or medication dose might need tweaking.
Regular follow-ups with your doctor are opportunities to fine-tune your plan. Experts recommend checking in every few months, or more often when trying new treatments. Your symptom journal is crucial for these conversations.
The goal isn’t to find one perfect treatment and stick with it forever. Long-term management is an ongoing conversation between you and your healthcare team.
Being an active participant in your care means speaking up, asking questions, and being honest about what’s working and what isn’t. Patient empowerment means recognizing you are the expert on your own body. Combining your expertise with your team’s medical knowledge is how real progress happens.
Conclusion: Taking Control of Your Fibromyalgia Pain
After exploring the pathways to fibromyalgia chronic pain relief, the main takeaway is that there is no single solution. Your journey to better health is unique and will involve combining different strategies until you find what brings you the most relief.
The most successful treatment plans weave together multiple strategies, such as gentle exercise, therapy, medication, acupuncture, or dietary changes. For some, medical cannabis is the breakthrough, while others thrive with physical therapy and mindfulness.
The key is patience with yourself and the process. Your symptoms can change, so your treatment plan should evolve too. Don’t give up hope—effective relief is possible.
I’ve seen patients transform their lives by staying open to new possibilities. The treatment that seemed unlikely can become a game-changer. Every option deserves consideration.
If you’re in Florida and decide to explore medical cannabis for your fibromyalgia chronic pain relief, you’ll find several qualified providers to guide you through the process of obtaining a medical marijuana card. Well-known clinics like Marijuana Doctor, CannaMD, and Miracle Leaf operate throughout the state. When choosing a provider, it’s helpful to compare factors like physician expertise in fibromyalgia, patient reviews, and the overall cost and ease of the process.
At Canna Doctors of America, we’re here to help. We provide professional, same-day consultations to determine if a medical marijuana card is right for you. Our team understands chronic pain and is committed to making your path to treatment as smooth as possible.
You don’t have to steer this alone. With locations in Tampa, St. Petersburg, and Clearwater, we make it easy to get the guidance you need. Take the next step in controlling your fibromyalgia pain—you deserve to feel better.
Ready to explore your options? Get more info about getting a medical card and start your journey toward better pain management today.